Thyroid cancer originates in the thyroid gland, a butterfly-shaped organ located at the base of the neck. This gland produces hormones that regulate metabolism, body temperature, blood pressure, and heart rate. While thyroid cancer is relatively uncommon, it is generally highly treatable with an excellent cure rate.
Types of Thyroid Cancer
– Papillary Thyroid Cancer:
The most prevalent form, accounting for approximately 80% of cases. It typically affects younger individuals and is more common in women. Papillary thyroid cancer usually grows slowly and often spreads to lymph nodes in the neck. Early detection leads to a high treatment success rate.
– Follicular Thyroid Cancer:
Comprises about 10-15% of thyroid cancers. It tends to occur in middle-aged adults and can spread to other body parts, such as bones and lungs.
– Medullary Thyroid Cancer
Accounts for approximately 2% of thyroid cancers. It arises from the thyroid’s C cells, which produce the hormone calcitonin. This type can be sporadic or associated with genetic syndromes.
– Anaplastic Thyroid Cancer:
A rare and aggressive form, making up about 1% of cases. It typically occurs in individuals over 60 and is challenging to treat due to its rapid growth and spread.
– Thyroid Lymphoma:
An uncommon type originating from the immune system cells within the thyroid gland. It usually presents in older adults and requires specialized treatment approaches.
Symptoms of Thyroid Cancer
Risk Factors
Several factors may increase the risk of developing thyroid cancer:
- Gender: Women are more susceptible than men.
- Age: While thyroid cancer can occur at any age, certain types are more common in specific age groups.
- Radiation Exposure: Previous exposure to high levels of radiation, particularly during childhood, increases risk.
- Family History: A family history of thyroid cancer or genetic syndromes can elevate risk.
- Iodine Deficiency: Lack of iodine in the diet has been linked to certain types of thyroid cancer.
Treatment Options
Treatment strategies are tailored based on the type and stage of thyroid cancer:
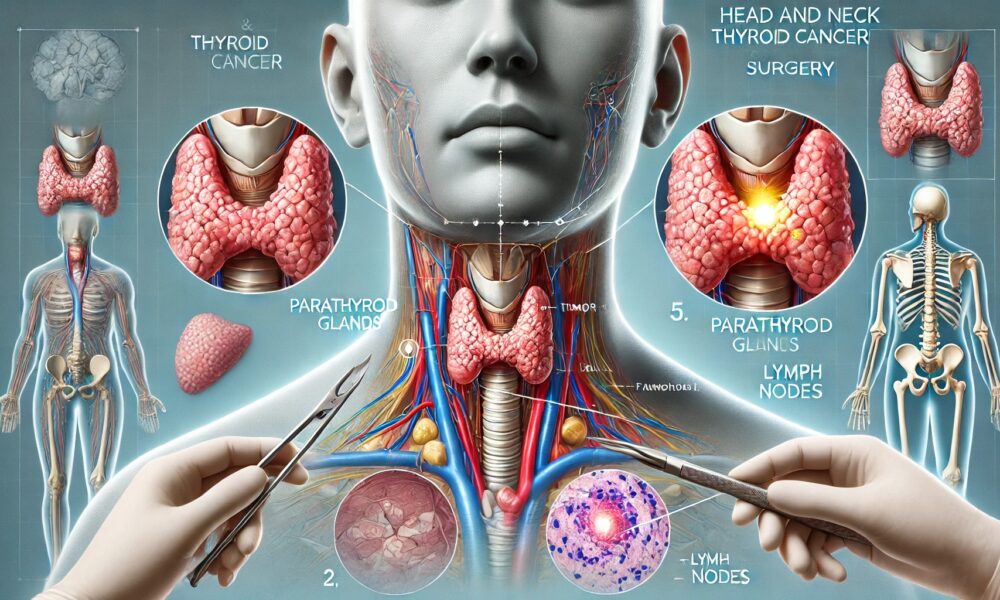
- Surgery: The primary treatment for most thyroid cancers involves removing part or all of the thyroid gland (thyroidectomy). Nearby lymph nodes may also be removed if the cancer has spread.
- Radioactive Iodine Therapy: Utilized after surgery to eliminate any remaining thyroid tissue or microscopic cancer cells. This treatment is particularly effective for papillary and follicular thyroid cancers.
- Thyroid Hormone Therapy: Prescribed to replace essential hormones and suppress the production of thyroid-stimulating hormone (TSH), which can promote cancer growth.
- External Radiation Therapy: Employed in cases where surgery isn’t an option or if cancer persists after other treatments.
- Chemotherapy: Generally reserved for advanced thyroid cancers unresponsive to other treatments.
- Targeted Therapy: Involves medications that specifically target cancer cell abnormalities, offering a treatment option for cancers that don’t respond to traditional therapies.
Diagnostic Approach
Early detection is crucial for effective treatment. Diagnostic methods include:
Physical Examination
✔ Assessing the neck for lumps or abnormalities.
Imaging Tests & Biopsy
✔ Fine-needle aspiration to obtain tissue samples for analysis.
Blood Tests
Prognosis
The outlook for thyroid cancer patients is generally favorable, especially when diagnosed early. Regular follow-ups are essential to monitor for recurrence and manage any long-term effects of treatment.
Preventive Measures
While not all cases are preventable, certain measures can reduce risk:
- Avoid Unnecessary Radiation: Limit exposure, particularly during childhood.
- Genetic Counseling: For those with a family history, counseling can provide insights into risk and preventive strategies.
- Adequate Iodine Intake: Ensuring sufficient iodine in the diet supports thyroid health.